WHO Fungal Identification in Hospital Environments
In healthcare settings, especially hospitals, fungal infections can pose significant risks to patients. Among these fungi, those recognized by the World Health Organization (WHO) are of particular concern due to their pathogenicity and potential for causing severe illnesses. Accurate identification of these pathogens is crucial for effective treatment strategies and infection control measures.
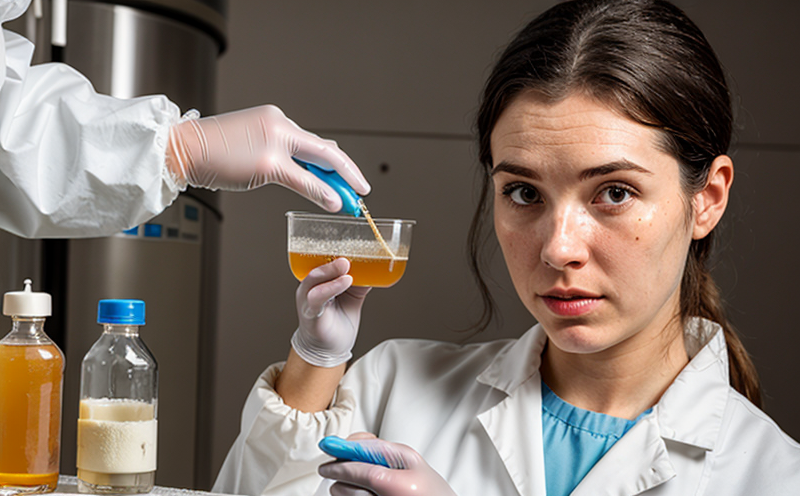
The process involves several steps, starting with the collection of specimens such as sputum, blood cultures, or tissue biopsies. Specimens are then cultured under controlled conditions to promote fungal growth, which can take anywhere from 1-3 weeks depending on the type of fungus. Once growth is observed, it's critical to differentiate between various species within the genus Candida and other medically important fungi like Aspergillus, Cryptococcus, and Fusarium.
Traditional methods for fungal identification include microscopic examination using stains (e.g., Calcofluor White), biochemical tests, and phenotypic characteristics. However, these approaches are often labor-intensive and may not be sufficiently sensitive or specific. Modern techniques like MALDI-TOF MS (Matrix-Assisted Laser Desorption/Ionization-Time of Flight Mass Spectrometry) offer faster results but require robust bioinformatics databases for accurate identification.
A key challenge in identifying these fungi lies in distinguishing between similar-looking species, particularly within the Candida genus. Misidentification can lead to inappropriate antifungal therapy, thereby increasing morbidity and mortality rates among patients suffering from invasive candidiasis or other systemic mycoses. This underscores the importance of employing advanced technologies that provide rapid yet precise identification.
In addition to clinical significance, accurate identification also supports epidemiological studies aimed at tracking outbreaks and understanding transmission patterns within healthcare facilities. By providing reliable data on the prevalence and distribution of specific fungal pathogens, laboratories contribute valuable insights towards improving patient safety practices across hospitals worldwide.
Industry Applications
| Application | Description |
|---|---|
| Clinical Diagnostics | Detecting and identifying pathogenic fungi in patient samples to guide appropriate treatment. |
| Outbreak Surveillance | Tracking the spread of fungal infections within healthcare facilities, enabling targeted interventions. |
| Epidemiological Research | Analyzing trends in fungal infections to inform public health policies and practices. |
| Antifungal Drug Development | Assisting pharmaceutical companies in developing new drugs targeting specific fungi identified in clinical samples. |
| Infection Control | Providing evidence-based information to healthcare providers for implementing effective infection control measures. |
| Public Health Monitoring | Contributing data towards national and international initiatives aimed at reducing fungal disease burdens globally. |
Quality and Reliability Assurance
The reliability of WHO fungal identification in hospital environments hinges on rigorous quality assurance protocols. These include using standardized reference materials, ensuring personnel are trained in current best practices, validating new methodologies against established standards, and maintaining up-to-date databases for accurate species differentiation.
ISO 15189:2012 provides guidelines for the establishment of clinical laboratories that ensure high standards of quality and reliability. Compliance with such international standards guarantees consistency in test outcomes across different institutions, enhancing confidence in diagnostic results.
To further enhance accuracy, laboratories should adhere to strict specimen handling procedures to minimize contamination risks during collection and transport. Additionally, regular calibration of instruments used in the identification process ensures precise measurements throughout testing cycles. Regular audits by independent bodies help maintain these high standards continuously.
Ensuring compliance with stringent quality assurance measures not only improves diagnostic accuracy but also fosters trust between healthcare providers, patients, and regulatory authorities. By adhering to these best practices, laboratories play a pivotal role in safeguarding public health while contributing positively to medical advancements.
Competitive Advantage and Market Impact
Offering WHO fungal identification services equips healthcare providers with essential tools necessary for combating fungal infections effectively. This capability sets them apart from competitors by offering comprehensive diagnostic solutions tailored specifically to the needs of their patients.
By leveraging advanced technologies like MALDI-TOF MS, laboratories demonstrate their commitment to staying at the forefront of medical science. Such investments signal both internal stakeholders and external partners that they prioritize innovation and excellence in every aspect of operations.
The ability to rapidly identify pathogenic fungi allows for quicker initiation of appropriate antifungal therapies, potentially reducing patient recovery times and associated costs. For hospitals seeking competitive advantages, investing in such services represents a strategic decision aimed at improving overall patient care quality and satisfaction levels.
In terms of market impact, providing accurate WHO fungal identification contributes significantly to broader public health initiatives. Reliable data generated through these tests informs policy decisions made by governments and international organizations working towards eradicating fungal diseases worldwide. Thus, participating in this service not only benefits individual institutions but also supports global efforts aimed at improving healthcare standards.