USP Pseudomonas aeruginosa Detection Testing
The USP Pseudomonas aeruginosa detection testing is a critical process in pharmaceutical quality assurance and compliance. This stringent test ensures that batches of active pharmaceutical ingredients (APIs) and finished dosage forms do not contain the opportunistic pathogen Pseudomonas aeruginosa. This bacterium can cause severe infections, especially in immunocompromised patients, and its presence is unacceptable in sterile products.
The testing protocol follows United States Pharmacopeia (USP) General Chapter Chapter 1127 for the Detection of Pseudomonas aeruginosa. This chapter provides detailed guidelines on how to perform this test, which is essential for ensuring product safety and quality.
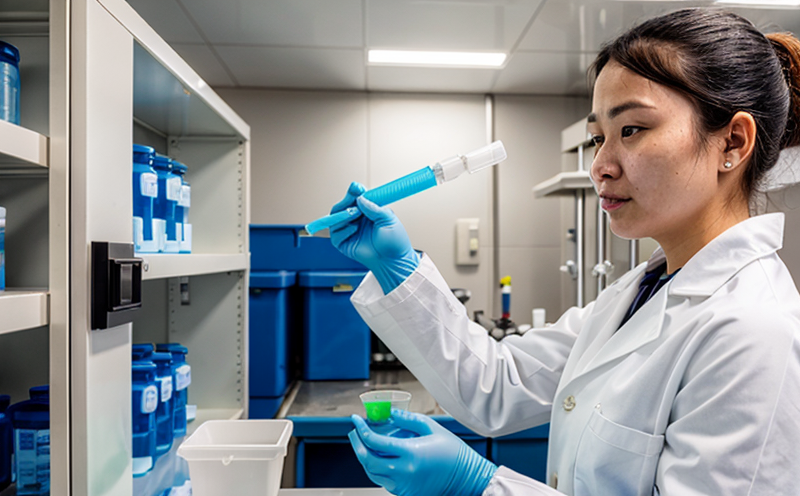
The testing process involves several key steps. First, a sterile sample is prepared from the pharmaceutical batch in question. This preparation ensures that any contamination introduced during sampling does not affect the integrity of the test results. The sample is then inoculated onto an appropriate culture medium, which supports the growth of Pseudomonas aeruginosa if it is present.
The medium used for this purpose is a nutrient-rich agar base that includes specific components to encourage the isolation and identification of pseudomonads. After incubation at 35°C to 37°C for 18 to 24 hours, the culture plates are inspected for colony morphology indicative of Pseudomonas aeruginosa. The bacterium is identified by its distinctive blue-greenish color on the agar and a metallic sheen when viewed under a microscope.
Once colonies suspiciously resembling those of Pseudomonas aeruginosa are observed, they undergo further testing. A Gram stain is performed to check for gram-negative rods, which is one of the initial criteria for this bacterium. Following this, biochemical tests like oxidase and indole reactions are conducted to confirm identification.
The importance of this test cannot be overstated in ensuring that pharmaceutical products meet stringent quality standards. The presence of Pseudomonas aeruginosa can lead to product recalls, legal issues, and damage to brand reputation. By adhering to USP guidelines, laboratories ensure that they provide the highest level of assurance regarding the safety and efficacy of pharmaceuticals.
In conclusion, the USP Pseudomonas aeruginosa detection testing is a vital component in maintaining the integrity and safety of pharmaceutical products. It underscores the commitment to quality and compliance required by regulatory bodies worldwide.
Applied Standards
The USP Pseudomonas aeruginosa detection test strictly adheres to the guidelines provided in USP Chapter 1127. This chapter outlines the methodology and acceptance criteria for detecting this bacterium. Compliance with these standards is mandatory to ensure accurate and reliable test results.
The standard specifies that the test should be conducted using a nutrient-rich agar medium, which includes components like peptone, yeast extract, and sodium chloride, designed specifically to support the growth of Pseudomonas aeruginosa. The incubation period is set at 18 to 24 hours at 35°C to 37°C. During this time, any colonies resembling those of Pseudomonas aeruginosa should be observed and analyzed.
The standard also requires the use of specific biochemical tests to confirm the identification of the bacterium. These include the oxidase test, which is positive for pseudomonads, and the indole test, which can differentiate between Pseudomonas aeruginosa and other similar organisms. Additionally, API strips or VITEK systems are often used for rapid identification.
The acceptance criteria for this test are stringent. Any colonies that exhibit the characteristic blue-green coloration and metallic sheen under a microscope must be further analyzed to confirm their identity as Pseudomonas aeruginosa. If any such colonies are found, they should not exceed certain acceptable limits specified in the USP guidelines.
By adhering strictly to these standards, laboratories ensure that their results are accurate and reliable, meeting the highest quality assurance requirements. This compliance is crucial for maintaining the integrity of pharmaceutical products and ensuring patient safety.
Scope and Methodology
The scope of USP Pseudomonas aeruginosa detection testing encompasses all stages from sample preparation to final confirmation. The process begins with the collection and preparation of a sterile sample from the pharmaceutical batch in question. This step is critical as any contamination introduced during sampling can skew test results.
Once prepared, the sample is inoculated onto a nutrient-rich agar medium that supports the growth of Pseudomonas aeruginosa. After incubation for 18 to 24 hours at 35°C to 37°C, the culture plates are inspected for colonies with characteristic blue-green color and metallic sheen. These features are indicative of pseudomonads.
The next step involves further identification using biochemical tests such as the oxidase test and indole reaction. The oxidase test is particularly significant as it differentiates Pseudomonas aeruginosa from other gram-negative rods by producing a positive result. This test, along with others like the API strips or VITEK systems, ensures accurate identification.
The methodology also includes using appropriate media and incubation conditions to maximize the chances of detecting pseudomonads if they are present in low numbers. The use of these specific methods is crucial for ensuring that the test results are both sensitive and specific.
Finally, the acceptance criteria are applied to determine whether the batch meets the required standards. Any colonies exhibiting the characteristic features must be counted and compared against acceptable limits set by USP guidelines. If the counts exceed these limits, further investigation is necessary to identify the source of contamination and ensure corrective measures are taken.
This comprehensive approach ensures that pharmaceutical batches meet stringent quality requirements, thereby enhancing product safety and reliability.
Benefits
The benefits of USP Pseudomonas aeruginosa detection testing extend beyond ensuring compliance with regulatory standards. This rigorous testing process plays a pivotal role in protecting patient health by preventing the introduction of harmful bacteria into pharmaceutical products.
First and foremost, this test helps to maintain product safety by eliminating the risk of contamination from Pseudomonas aeruginosa. The presence of this bacterium can lead to severe infections, particularly in immunocompromised patients. By detecting its presence early on, laboratories can prevent such risks and ensure that only safe products reach the market.
Secondly, compliance with USP guidelines enhances brand reputation by demonstrating a commitment to quality and patient safety. This adherence to strict standards builds trust among healthcare professionals and consumers, reinforcing the integrity of pharmaceutical brands.
The test also aids in maintaining regulatory compliance. Regulatory bodies like the FDA and EMA rely on consistent testing methods to ensure that all pharmaceutical products meet stringent safety and efficacy criteria. By using USP Pseudomonas aeruginosa detection testing, laboratories can avoid non-compliance issues that could lead to product recalls or legal challenges.
In addition, this testing process supports the development of new drugs by ensuring that they undergo rigorous quality control measures from the earliest stages of production. This ensures that even experimental and investigational products meet high-quality standards before being introduced into clinical trials or market release.
Finally, the test benefits healthcare professionals by providing accurate information on product safety. This enables them to prescribe medicines confidently, knowing that they comply with international standards. Such transparency enhances patient trust in both pharmaceutical companies and healthcare providers.
In summary, USP Pseudomonas aeruginosa detection testing is a vital tool for ensuring the safety, efficacy, and integrity of pharmaceutical products. It supports compliance with regulatory standards, protects patients from harmful bacteria, and reinforces brand reputation through consistent quality assurance practices.